Student Health & Counseling strives to provide quality health care and wellness services in an environment that is non-judgemental and respectful of each individual as well as their privacy. Our staff strives to be sensitive to the issues of those who may be sexually active.
SHCS provides consultation, evaluation, treatment, as well as educational and support resources to promote optimal health.
-
-
SHCS provides care and treatment of health concerns unique to being male†. Our providers work to provide our patients with a supportive, confidential and non-judgmental environment in where they can ask questions and discuss concerns.
Available Services for Men’s Health:- Evaluation and treatment for sexual health issues
- Check-up, diagnosis and treatment of sexually transmitted infections and diseases‡
- HIV Testing
- Support in maintaining sexual health
- Support and assistance for concerns relating to sexual function or performance
- Support and assistance for concerns relating to sexual orientation
- Information about testicular self exams
- Routine age-specific laboratory testing
- Blood pressure screening
- Review of medication
- Information about diet and exercise
- *Services described on this page might be relevant for students with a variety of gender identities, including ciswomen, transmen, transwomen and gender non-conforming people. Members of SHCS are currently working to make this language more inclusive. We appreciate your patience, support and input.
†including transwomen or gender non-conforming students with a penis.
‡Important information on STD screening: A urine test is a simple, but reliable way of detecting infections of the urethra in men. To do this, you must not urinate for at lease three hours prior to giving your specimen, and it is important that only the initial 10cc (marked on the container) of your stream be collected.
-
-
-
Student Health & Counseling provides confidential information, examinations, and treatment, and information regarding all women's* health issues. Our staff includes physicians and nurse practitioners who specialize in women's health.
Available Services for Women’s† Health:- Evaluation and treatment for sexual health issues
- Check-up, diagnosis and treatment of sexually transmitted infections and diseases‡
- HIV Testing
- Support in maintaining sexual health
- Support and assistance for concerns relating to sexual function or performance
- Support and assistance for concerns relating to sexual orientation
- Information about testicular self exams
- Routine age-specific laboratory testing
- Blood pressure screening
- Review of medication
- Information about diet and exercise
- *including transmen or gender non-conforming students with a cervix.
†Services described on this page might be relevant for students with a variety of gender identities, including ciswomen, transmen, transwomen and gender non-conforming people. Members of SHCS are currently working to make this language more inclusive. We appreciate your patience, support and input.
‡Important information on STD screening: A urine test is a simple, but reliable way of detecting infections of the urethra in men. To do this, you must not urinate for at lease three hours prior to giving your specimen, and it is important that only the initial 10cc (marked on the container) of your stream be collected.
-
-
To inquire about Plan B, please walk-in to SHCS. Plan B, the "morning after pill", may be used after having unprotected sex to guard against unwanted pregnancy. Plan B works better the sooner you use it and needs to be taken within 72 hours of unprotected intercourse or contraceptive failure. For more information on Plan B, see Plan B Frequently Asked Questions.
-
-
-
The affordability, availability, efficacy, and safety of contraception has greatly benefited women's health. With the many different forms of birth control available to women today, the decision about which type is best suited for an individual woman can be confusing and dependent on on many variables, including past medical history, ease of use, incidence of side effects, cost and risks. Our providers are specialists in all forms of contraception and can offer advice as to which option may be the best for you. Schedule an appointment with a provider by calling 415-476-1281 or by visiting myhealthrecord.ucsf.edu.
-
-
-
-
Annual PAP exams may be done at SHCS or you may choose an OB-GYN once every 12 months provided you notify Student Health. Notification is necessary to ensure your visit will be paid by Anthem.
-
-
-
-
-
Condoms are barrier methods that prevent the deposit of sperm and other body fluids into the orifice being penetrated during penis-vagina, penis-anus, or penis-mouth sex. Condoms are the only contraceptive method that also protect against STIs, with the exception of animal skin condoms, which do not offer such protection.
Two types of condoms are currently available: traditional and insertive.
SHCS offers 'traditional' condoms at a discounted price of $2.00 for a dozen or $5.00 for three dozen.
SHCS offers 'insertive' condoms (FC2) for free while supplies last.
Stop by either the Parnassus or Mission Bay clinic to purchase.
- A traditional condom consists of a thin sheath of latex or polyurethane worn on the penis, but may also be worn on a sex toy or phallus shaped object. With perfect use, a traditional condom is 98% effective at preventing pregnancy; with typical use, it is 85% effective.
- The insertive condom is commonly known as the female condom, but it can also be used for penis/toy-anus, penis/toy-vagina sex. Insertive condoms are made of nitrile, making them a great option for anyone with a latex sensitivity or allergy. They are 95% effective for preventing pregnancy with perfect use, and 79% effective with typical use.
-
-
-
The contraceptive injection is a shot that contains the hormone progesterone. This hormone stops your body from releasing eggs and thickens the mucus at the cervix. You need one shot every three months from a healthcare provider. Once injected, it is not reversible, i.e. in case of side effects it cannot be stopped. The way it works is similar to the pill, or the ring, except you don’t have to remember to take it every day or week.
When you stop the shot it may take your period up to one year to return to normal. Prolonged (longer than 2 years) of use may affect your bone density, it may cause weight gain and it does not protect against STIs.
-
-
-
For a new prescription, or to transfer an existing prescription if you’ve never been seen at UCSF SHCS, schedule an appointment with your SHCS primary care provider. SHCS providers can provide pills if you do or do not have UC SHIP insurance. To get refills of a prescription you previously obtained at SHCS please have your pharmacy message your provider.
-
-
-
SHCS providers are trained to both counsel and place a Mirena IUD for patients.
An IUD is a small device shaped like a “T”. Your health care provider places it in your uterus during an office visit.
There are three IUDs available in the US: Paraguard, Kyleena, and Mirena. The Paraguard IUD contains copper and is effective for up to 10 years. The copper prevents fertilization by reducing the motility of sperm which prevents them from getting to the egg. Mirena and Skyla contain a progestin hormone, levonorgrestrel. The Kyleena is effective for 3 years, Mirena for 5 years. Progestin thickens the cervical mucus and the lining of the uterus, temporarily causing atrophy of the endometrium, inhibiting sperm entrance and movement into the uterus or fallopian tube. The Mirena may also be prescribed to control heavy periods for women who do not need contraception. Mirena and Kyleena do not contain estrogen. For some women a contraceptive without estrogen is important. All 3 IUDs are equally effective for contraception.
All IUDs have a thin string attached at the base of the “T”. This allows your health care provider to remove the IUD in the office and for you to check to make sure the IUD is in your uterus.IUDs are as effective as tubal ligations (getting your tubes tied) – but unlike a tubal ligation an IUD is completely reversible, and more effective than birth control pills. Annually, less than one IUD user in a hundred gets pregnant. Once the IUD is placed, there is nothing you have to do to make it work. Once inserted, you and your partner should not feel it. The Mirena IUD has the added benefits of decreasing menstrual cramps and anemia.
Once an IUD is removed you can become pregnant immediately so if you do not desire pregnancy you must use birth control after removal.
To inquire about an IUD placement, please call SHCS at (415) 476-1281 and schedule an appointment.
-
-
-
Schedule an appointment with a SHCS provider to learn more and/or be fit for a diaphragm.
-
-
-
-
-
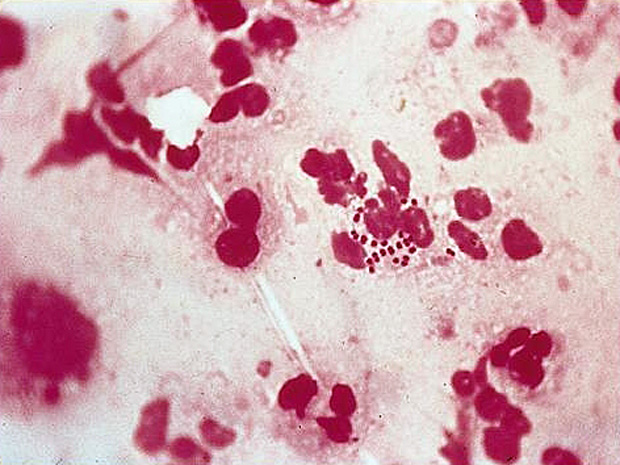
Where: Moist areas; cervix, uterus, fallopian tubes, throat, mouth, & anus
Risk: Sexual contact with an infected partner; Untreated can cause Pelvic Inflammatory Disease
Symptoms: Men: white, yellow, green discharge, painful testicles;
Females: unusual discharge, painful urination
Treatment: Antibiotics
Prevention: Informed choices between partners; Consistent use of latex condoms
More info can be found here.
-
-
-
Risk: Any sexual activity with an infected person; Known as the silent infection because most don’t know they have it & in women it can cause Pelvic Inflammatory Disease
Symptoms: Abnormal discharge
Treatment: Antibiotics
Prevention: Informed choices between partners; Consistent use of latex condoms
More info can be found here.
-
-
-

Risk: Person to person by direct contact with syphilis sores mainly on the genitals, vagina, anus, or in the rectum
Symptoms: 1° stage: a single sore lasting 3-6 wks;
2° stage: rough, red/brown rash on palms or soles of feet; rashes, sores of mouth, vagina, or anus; Latent: no symptoms;
Late stage: damage of internal organs
Treatment: Antibiotics
Prevention: Informed choices between partners; Consistent use of latex condoms
More info can be found here.
-
-
-
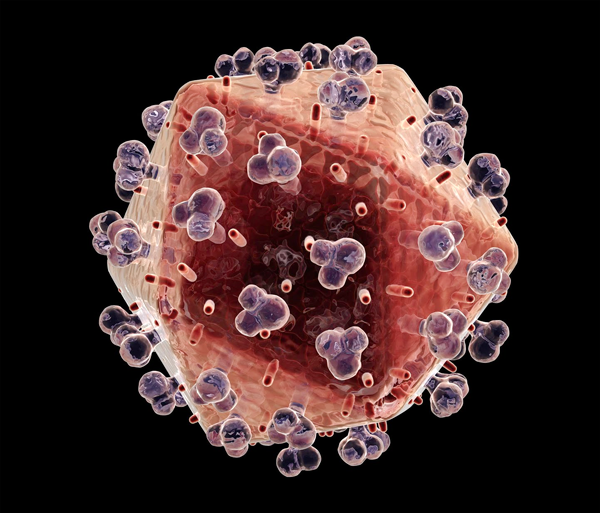
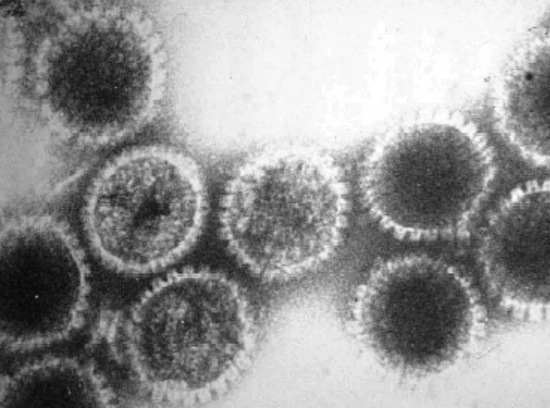
What: HIV is the Human Immunodeficiency Virus. It is the virus that can lead to acquired immune deficiency syndrome, or AIDS. Acquired Immunodeficiency Syndrome , or AIDS, is the late stage of HIV infection, when a person’s immune system is severely damaged and has difficulty fighting diseases and certain cancers. With the advent of “highly-active” drug combinations, people can live much longer - even decades - with HIV before they develop AIDS
Risk: HIV is spread primarily by: • Not using a condom when having sex with a person who has HIV
• Having multiple sex partners or the presence of other sexually transmitted diseases (STDs) can increase the risk of infection during sex
• Sharing needles, syringes, rinse water, or other equipment used to prepare illicit drugs for injection.
• Being born to an infected mother—HIV can be passed from mother to child during pregnancy, birth, or breast-feeding.
Symptoms: Within a few weeks of being infected with HIV, some people develop flu-like symptoms that last for a week or two, but others have no symptoms at all.
Treatment: Obtain medical treatment immediately if you think you were exposed to HIV. HIV medications can prevent infection if they are started quickly. If you’ve been diagnosed w/ HIV, continue on your prescribed treament plan and check in with your provider regularly.
Prevention: Because the most common ways HIV is transmitted is through anal or vaginal sex or sharing drug injection equipment with a person infected with HIV, know your status and the status of your partner. Everyone between the ages of 13 and 64 should be tested for HIV at least once. If you are at increased risk for HIV, you should be tested for HIV at least once a year; Limit your number of sex partners or be in a long-term mutually monogamous relationship with an uninfected partner. The fewer partners you have, the less likely you are to encounter someone who is infected with HIV or another STD; Correct and consistent condom use. Latex condoms are highly effective at preventing transmission of HIV and some other sexually transmitted diseases.“Natural” or lambskin condoms do not provide sufficient protection against HIV infection.; Do not inject drugs. If you do inject drugs, do not share needles and use clean needles and works
More info can be found here.
-
-
-
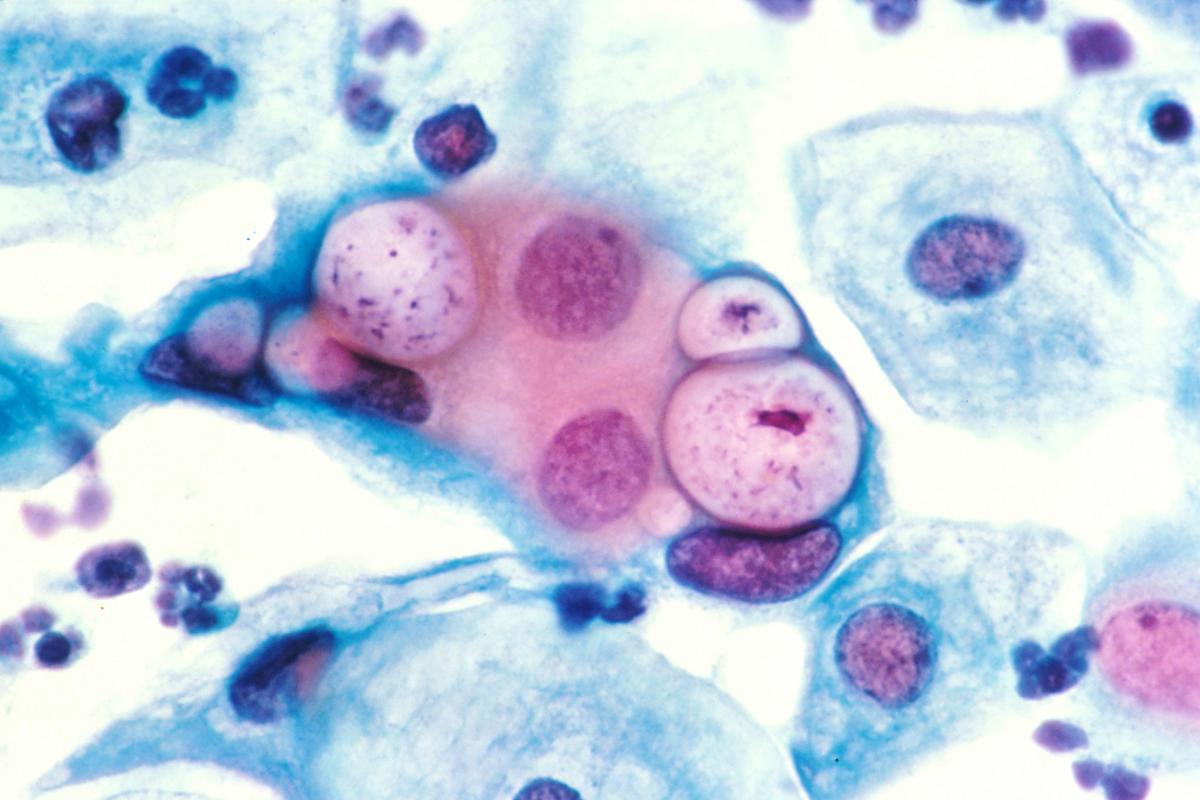
What: Transmitted by herpes simplex virus type 1 (HSV-1) or type 2 (HSV-2). 1 in 6 people have a form of herpes
Risk: Sexual contact (oral or genital) with an infected partner
Symptoms: Most have no symptoms; Sometimes one or more painful sores around genitals, rectum, or mouth that take 2-4 weeks to heal
Treatment: Herpes cannot be cured, but you can take antiviral medication to reduce symptoms of sores
Prevention: Informed choices between partners; Consistent use of latex condoms
More info can be found here.
-
-
-

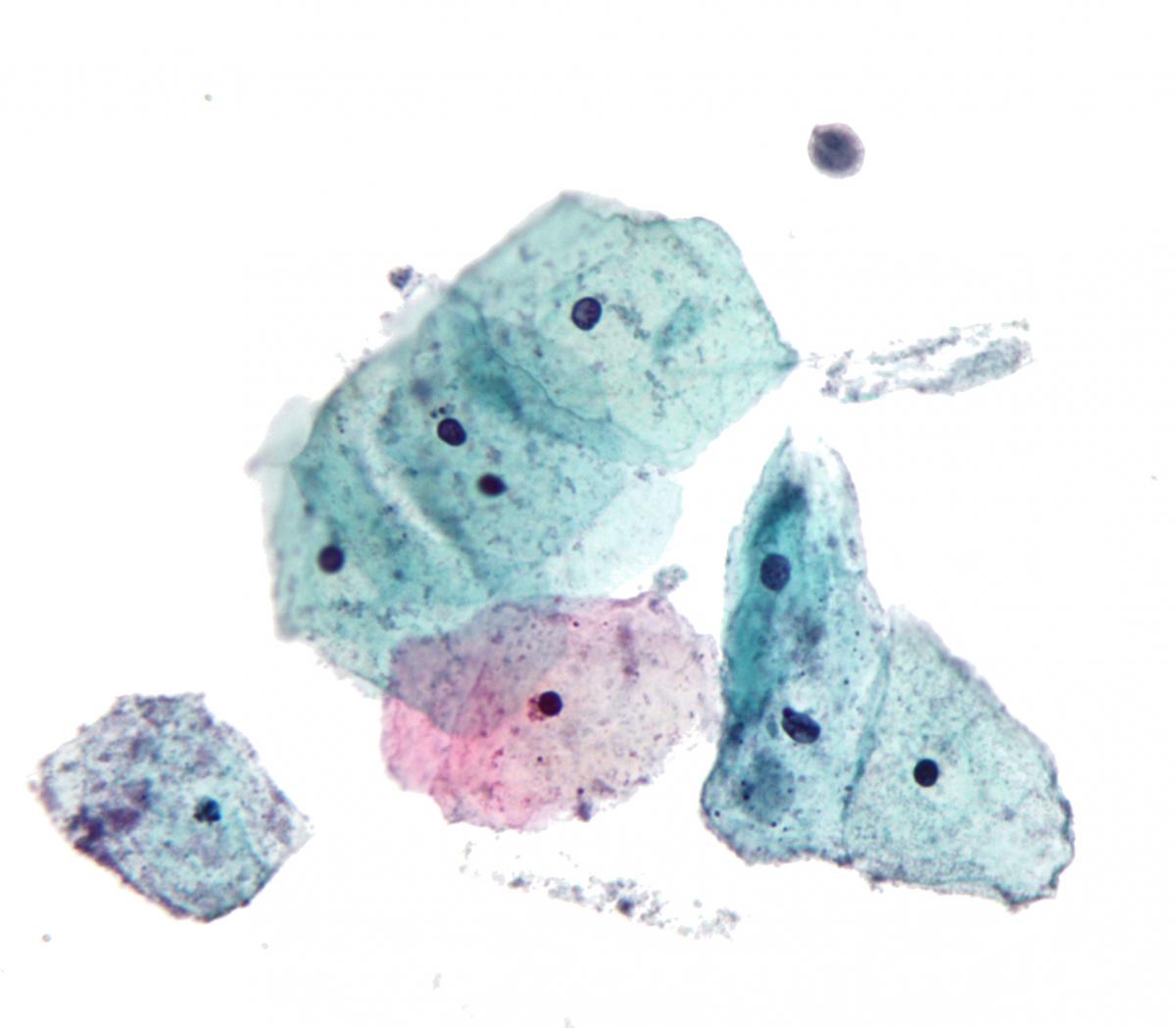
Risk: Person to person by direct genital contact
Symptoms: Genital Warts: Small bump or group of bumps, raised or flat, or shaped like cauliflower.
Cervical Cancers: No symptoms until it’s in advanced stages.
Treatment: No treatment for virus, but are for health problems associated w/ HPV
Prevention: HPV Vaccines for females & males ages 13-26 years old can lower the chances of getting HPV; Regular screening for women; Informed choices between partners; Consistent use of latex condoms
More info can be found here.
-
-
-
What: Caused by infection with a protozoan parasite called trichmonas vaginalis
Risk: Sexual contact with an infected partner
Symptoms: Men may be carriers, but women are more likely to show symptoms. Symptoms may range from mild irritation to severe inflammation of vagina between 5-28 days after exposure
Treatment: Trichomoniasis can be cured with a single dose of prescription antibiotic medication (either metronidazole or tinidazole)
Prevention: Informed choices between partners; Consistent use of latex condoms
More info can be found here.
-
-
-
-
The University of California is committed to creating and maintaining a community where all persons who participate in University programs and activities can work and learn together in an atmosphere free of all forms of harassment, exploitation, or intimidation. Every member of the University community should be aware that the University prohibits sexual harassment and sexual violence, and that such behavior violates both law and University policy. The University will respond promptly and effectively to reports of sexual harassment and sexual violence, and will take appropriate action to prevent, to correct, and when necessary, to discipline behavior that violates this policy on Sexual Harassment and Sexual Violence This policy applies to all University employees and students.This Policy applies to the University of California campuses, the Lawrence Berkeley National Laboratory, the Medical Centers, and the Office of the President, and all auxiliary University locations
Consent, as referenced in this context, means:
- Consent is informed. Consent consists of an affirmative, conscious decision by each participant to engage in mutually agreed-upon sexual activity. Consent to some form of sexual activity does not imply consent to other forms of sexual activity.
- Consent is voluntary. It is given without coercion, force, threats, or intimidation; - it is a positive cooperation in the act or expression of intent to engage in the act pursuant to an exercise of free will.
- Consent is given when the person is not impaired or incapacitated. A person cannot consent if s/he is unconscious or coming in and out of consciousness. A person cannot consent if s/he/they is under the threat of violence, bodily injury or other forms of coercion, or has a mental disorder, developmental disability, or physical disability that would impair his/her/their understanding of the act.
- (a) Incapacitation is the physical and/or mental inability to make informed, rational judgments. States of incapacitation include, but are not limited to unconsciousness, sleep and blackouts.
- (b) Where alcohol or drugs are involved, incapacitation is distinct from drunkenness or intoxication, and is defined with respect to how the alcohol or other drugs consumed impacts a person’s decision-making capacity, awareness of consequences, and ability to make fully informed judgments. The factors to be considered include whether the accused knew, or a reasonable person in the position of the accused should have known, that the complainant was impaired or incapacitated
-
-
Sexual Harassment is unwelcome sexual advances, requests for sexual favors, and other verbal, nonverbal, or physical conduct of a sexual nature, when submission to or rejection of this conduct explicitly or implicitly affects a person’s employment or education, unreasonably interferes with a person’s work or educational performance, or creates an intimidating, hostile or offensive working or learning environment. Sexual harassment includes sexual violence. In the interest of preventing sexual harassment and sexual violence, the University will respond to reports of any such conduct.
Sexual harassment may include incidents between any members of the University community, including faculty and other academic appointees, staff, coaches, residents and interns, students, student employees (when acting within the course and scope of employment), and non-student or non-employee participants in University programs, such as vendors, contractors, visitors, and patients. Sexual harassment may occur in hierarchical relationships or between peers, or between persons of the same sex or opposite sex. In determining whether the reported conduct constitutes sexual harassment, consideration shall be given to the record of the conduct as a whole and to the totality of the circumstances, including the context in which the conduct occurred.
Consistent with the University of California Policies Applying to Campus Activities,Organizations, and Students, Policy 100.00 on Student Conduct and Discipline, Section102.09, harassment of one student by another is defined as unwelcome conduct of asexual nature that is so severe and/or pervasive, and objectively offensive, and that so substantially impairs a person’s access to University programs or activities that the person is effectively denied equal access to the University’s resources and opportunities.
-
-
-
Sexual Violence is defined as physical sexual acts perpetrated against a person’s will or where a person is incapable of giving consent. This includes: sexual assault, rape, battery, and sexual coercion; domestic violence; dating violence; and stalking.
- Domestic Violence is defined as abuse committed against an adult or a minor who is a spouse or former spouse, cohabitant or former cohabitant, or someone with whom the abuser has had a child or is having or has had a dating or engagement relationship.
- Dating Violence is defined as abuse committed by a person who is or has been in a social relationship of a romantic or intimate nature with the victim.
- Sexual Assault occurs when physical sexual activity is intentionally engaged in without the consent of the other person. The conduct may include physical force, violence, threat, or intimidation; ignoring the objections of the other person; causing the other person’s intoxication or impairment through the use of drugs or alcohol; taking advantage of the other person’s incapacitation(including voluntary intoxication), state of intimidation, or other inability to consent.
- Stalking is behavior in which a person repeatedly engages in a course of conduct directed at another specific person, that places that person in reasonable fear of their safety or the safety of a third person or persons.
-
-